Herpes is a common viral infection caused by the herpes simplex virus (HSV), which exists in two distinct types: Herpes Simplex Virus Type 1 (HSV-1) and Herpes Simplex Virus Type 2 (HSV-2). While both types can cause sores and blisters, they often affect different areas of the body and have unique characteristics. Understanding the differences between herpes 1 and herpes 2 is essential for effective management, treatment, and prevention of the virus.
The prevalence of herpes infections is widespread, with millions of individuals affected worldwide. HSV-1 is primarily associated with oral infections, leading to cold sores or fever blisters around the mouth, whereas HSV-2 is predominantly linked to genital infections. However, it's important to note that both types can cause infections in either location, complicating the diagnosis and treatment process. Herpes infections can be recurrent, with some individuals experiencing frequent outbreaks, while others may have asymptomatic infections.
In this comprehensive article, we will delve into the nuances of herpes 1 vs herpes 2, exploring their causes, symptoms, transmission methods, diagnosis, treatment options, and preventive measures. By gaining a thorough understanding of these two viral infections, individuals can make informed decisions about their health and well-being, minimizing the risk of transmission and managing outbreaks effectively.
Read also:Effortless Electrolysis Hair Removal At Home The Ultimate Guide
Table of Contents
- What is Herpes?
- Causes of Herpes
- Symptoms of Herpes
- How is Herpes Transmitted?
- Herpes 1 vs Herpes 2: What are the Differences?
- Diagnosing Herpes
- Treatment Options for Herpes
- Living with Herpes
- Preventing Herpes Transmission
- Herpes and Pregnancy
- Myths and Misconceptions About Herpes
- Emotional and Psychological Impact of Herpes
- Herpes in the Modern World
- Frequently Asked Questions About Herpes
- Conclusion
What is Herpes?
Herpes is a lifelong viral infection caused by the herpes simplex virus (HSV). The virus is categorized into two main types: HSV-1, which typically causes oral herpes, and HSV-2, which is more commonly associated with genital herpes. Both types of herpes can cause sores, blisters, and lesions on the skin and mucous membranes, leading to discomfort and pain during outbreaks.
Herpes is highly contagious and can be transmitted through direct contact with an infected person's skin or bodily fluids. The virus can remain dormant in the body for long periods, with outbreaks triggered by various factors such as stress, illness, or a weakened immune system. It's important to note that herpes infections can be asymptomatic, meaning an individual may carry and transmit the virus without exhibiting any noticeable symptoms.
While there is currently no cure for herpes, antiviral medications can help manage symptoms, reduce the frequency of outbreaks, and minimize the risk of transmission to others. With appropriate care and management, individuals with herpes can lead healthy and fulfilling lives.
Causes of Herpes
The primary cause of herpes infections is the herpes simplex virus, which exists in two types: HSV-1 and HSV-2. Herpes is typically transmitted through direct contact with an infected person's skin, mucous membranes, or bodily fluids. This can occur through various means, including:
- Oral contact, such as kissing or sharing utensils, leading to oral herpes (HSV-1).
- Sexual contact, including vaginal, anal, and oral sex, leading to genital herpes (HSV-2).
- Contact with an infected person's sores or blisters.
- Transmission from a mother to her baby during childbirth.
It's important to note that herpes can be transmitted even when an infected individual is asymptomatic, as the virus can be present on the skin without causing visible sores or blisters. Factors that can trigger herpes outbreaks include stress, illness, fatigue, and a weakened immune system.
Symptoms of Herpes
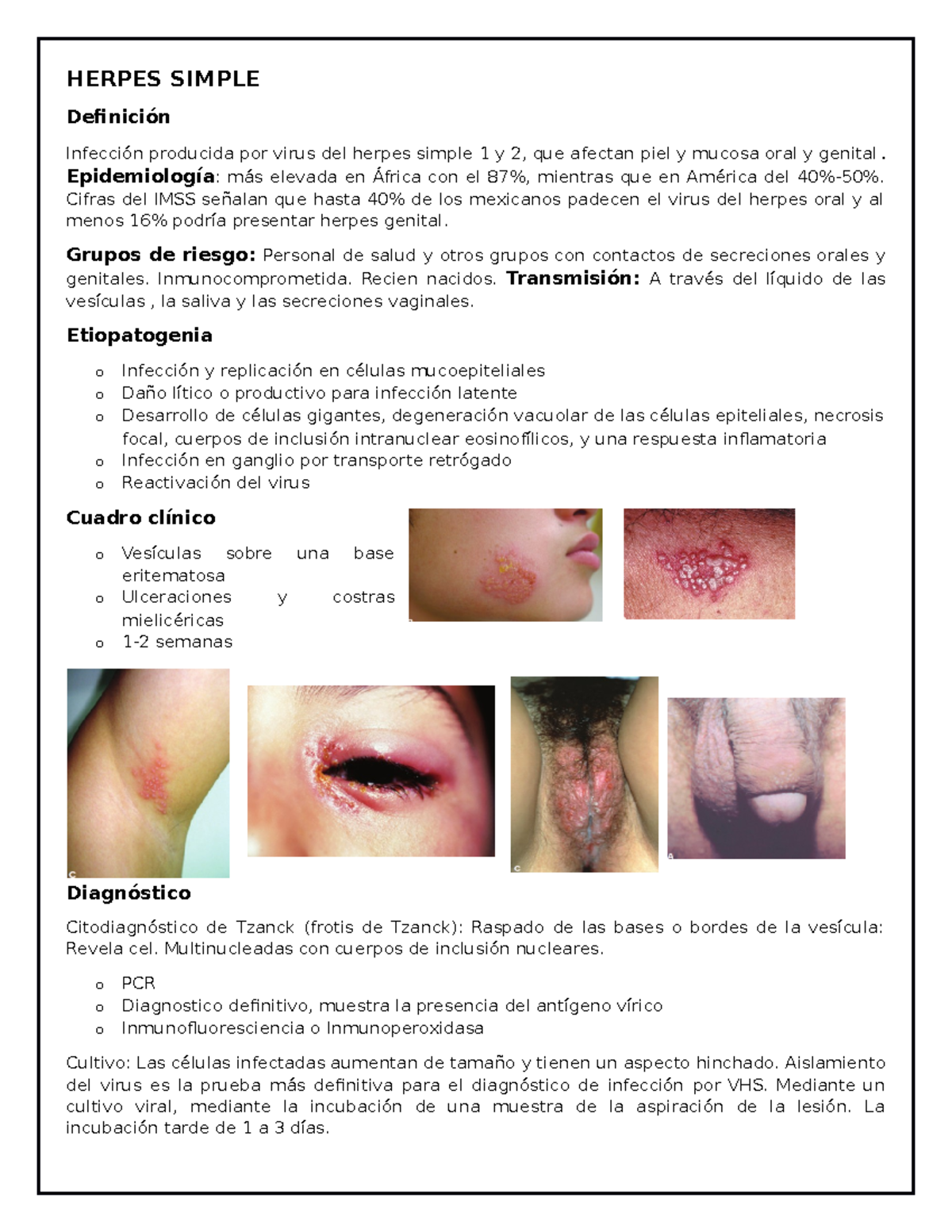
Herpes infections can present a range of symptoms, which may vary depending on the type of virus and the location of the infection. Common symptoms associated with herpes include:
Read also:Ultimate Guide To It Cosmetics Foundation A Smooth Skin Savior
- Blisters or sores on the mouth, lips, genitals, or other areas of the body.
- Itching, burning, or tingling sensations at the site of the infection.
- Pain or discomfort during urination (in the case of genital herpes).
- Fever, swollen lymph nodes, and body aches (during initial outbreaks).
- Recurrent outbreaks, with periods of remission between episodes.
It's important to note that some individuals may experience mild or no symptoms at all, making it challenging to diagnose herpes without medical testing. If you suspect you have herpes or are experiencing recurrent sores or blisters, it's essential to seek medical advice for proper diagnosis and treatment.
How is Herpes Transmitted?
Herpes is primarily transmitted through direct contact with an infected person's skin or bodily fluids. The virus can be spread through various means, including:
- Oral contact, such as kissing or sharing personal items like utensils or lip balm.
- Sexual contact, including vaginal, anal, and oral sex, with an infected partner.
- Touching an infected person's sores, blisters, or lesions.
- Transmission from a mother to her baby during childbirth.
It's important to note that herpes can be transmitted even when an infected individual is asymptomatic or not experiencing an outbreak. The virus can be present on the skin without causing visible sores, making it possible to spread the infection unknowingly. Practicing safe sex, avoiding sharing personal items, and seeking medical advice if you suspect an infection can help reduce the risk of transmission.
Herpes 1 vs Herpes 2: What are the Differences?
While both HSV-1 and HSV-2 are part of the herpes simplex virus family and share some similarities, they have distinct characteristics and differences that are important to understand:
Location of Infection
HSV-1 is primarily associated with oral infections, leading to cold sores or fever blisters around the mouth and lips. However, it can also cause genital infections through oral-genital contact. On the other hand, HSV-2 is predominantly linked to genital infections, causing sores or blisters in the genital and anal areas. Despite these distinctions, both types of herpes can infect either location, complicating the diagnosis and treatment process.
Transmission Methods
Both HSV-1 and HSV-2 are highly contagious and can be transmitted through direct contact with an infected person's skin, mucous membranes, or bodily fluids. HSV-1 is often spread through oral contact, such as kissing, while HSV-2 is primarily transmitted through sexual contact. It's important to note that both types of herpes can be spread even when an individual is asymptomatic, as the virus can be present on the skin without causing visible symptoms.
Symptoms and Outbreaks
The symptoms of herpes infections can vary depending on the type of virus and the location of the infection. HSV-1 typically causes oral sores, such as cold sores or fever blisters, while HSV-2 often leads to genital sores or blisters. Both types of herpes can cause recurrent outbreaks, with periods of remission between episodes. Factors that can trigger outbreaks include stress, illness, fatigue, and a weakened immune system.
Diagnosis and Treatment
Diagnosing herpes involves a combination of clinical examination, laboratory testing, and medical history evaluation. While there is no cure for herpes, antiviral medications can help manage symptoms, reduce the frequency of outbreaks, and minimize the risk of transmission to others. Both HSV-1 and HSV-2 can be managed effectively with appropriate care and treatment.
Diagnosing Herpes
Diagnosing herpes involves a combination of clinical examination, laboratory testing, and medical history evaluation. If you suspect you have herpes or are experiencing recurrent sores or blisters, it's essential to seek medical advice for proper diagnosis and treatment. The diagnostic process may include:
- Physical examination of sores, blisters, or lesions on the skin or mucous membranes.
- Swab tests, which involve collecting a sample from an active sore or blister for laboratory analysis.
- Blood tests to detect the presence of herpes antibodies in the bloodstream, indicating a past or current infection.
- Evaluation of medical history and symptoms to determine the likelihood of a herpes infection.
Accurate diagnosis is crucial for effective management and treatment of herpes infections. If you suspect you have herpes, it's important to seek medical advice and undergo appropriate testing to confirm the diagnosis.
Treatment Options for Herpes
While there is currently no cure for herpes, antiviral medications can help manage symptoms, reduce the frequency of outbreaks, and minimize the risk of transmission to others. Common treatment options for herpes include:
- Antiviral medications, such as acyclovir, valacyclovir, and famciclovir, which help reduce the severity and duration of outbreaks.
- Over-the-counter topical creams or ointments to alleviate pain, itching, and discomfort during outbreaks.
- Prescription pain relievers or numbing agents to manage pain and discomfort associated with sores or blisters.
- Lifestyle modifications, such as stress reduction, adequate rest, and a healthy diet, to support the immune system and reduce the risk of outbreaks.
Effective management of herpes involves a combination of medical treatment, lifestyle changes, and preventive measures to minimize the impact of the virus on daily life. If you have herpes, it's important to work closely with your healthcare provider to develop a personalized treatment plan that meets your specific needs.
Living with Herpes
Living with herpes can present challenges, but with appropriate management and support, individuals can lead healthy and fulfilling lives. Key considerations for living with herpes include:
- Adhering to prescribed antiviral medications and treatment plans to manage symptoms and reduce the frequency of outbreaks.
- Practicing safe sex and open communication with sexual partners to minimize the risk of transmission.
- Implementing lifestyle changes, such as stress reduction, adequate rest, and a healthy diet, to support the immune system and reduce the risk of outbreaks.
- Seeking support from healthcare providers, support groups, or counseling services to address emotional and psychological aspects of living with herpes.
By taking proactive steps to manage the virus and prioritize overall well-being, individuals with herpes can maintain a high quality of life and minimize the impact of the virus on their daily activities.
Preventing Herpes Transmission
Preventing the transmission of herpes involves a combination of safe practices and open communication with sexual partners. Key strategies for minimizing the risk of transmission include:
- Using condoms or dental dams during sexual activity to reduce the risk of transmitting the virus.
- Avoiding sexual contact during active outbreaks or when experiencing symptoms of herpes.
- Communicating openly with sexual partners about herpes status and potential risks.
- Practicing good hygiene, such as washing hands and avoiding sharing personal items like towels or razors.
By implementing these preventive measures, individuals can help reduce the risk of spreading the virus and protect both themselves and their partners from infection.
Herpes and Pregnancy
Herpes can pose risks during pregnancy, particularly if the mother experiences an outbreak near the time of delivery. Transmission of the virus from mother to baby during childbirth can lead to neonatal herpes, a serious condition that requires immediate medical attention. To reduce the risk of transmission during pregnancy, healthcare providers may recommend:
- Antiviral medications to manage symptoms and reduce the risk of outbreaks during pregnancy.
- Cesarean delivery (C-section) if active sores are present during labor, to prevent transmission to the baby.
- Close monitoring of the mother's health and any signs of herpes infection throughout the pregnancy.
If you are pregnant and have herpes, it's important to work closely with your healthcare provider to develop a comprehensive care plan that prioritizes the health and safety of both you and your baby.
Myths and Misconceptions About Herpes
Herpes is often surrounded by myths and misconceptions that can contribute to stigma and misinformation. Some common myths include:
- Myth: Herpes is a rare or uncommon infection.
- Reality: Herpes is a widespread and common infection, affecting millions of individuals worldwide.
- Myth: Herpes can only be transmitted during active outbreaks.
- Reality: Herpes can be transmitted even when an individual is asymptomatic, as the virus can be present on the skin without causing visible symptoms.
- Myth: Herpes is a sign of promiscuity or poor hygiene.
- Reality: Herpes can affect anyone, regardless of their sexual behavior or hygiene practices. It is a viral infection that can be transmitted through direct contact with an infected person's skin or bodily fluids.
By debunking these myths and promoting accurate information about herpes, individuals can make informed decisions about their health and well-being and reduce the stigma associated with the virus.
Emotional and Psychological Impact of Herpes
Living with herpes can have emotional and psychological implications, including feelings of shame, anxiety, or depression. It's important to address these aspects of the virus by:
- Seeking support from healthcare providers, support groups, or counseling services.
- Educating oneself about the virus to reduce fear and misconceptions.
- Practicing self-care and stress-reduction techniques to support mental well-being.
- Communicating openly with trusted individuals about the emotional impact of living with herpes.
By acknowledging and addressing the emotional and psychological aspects of herpes, individuals can develop healthy coping strategies and maintain a positive outlook on life.
Herpes in the Modern World
In the modern world, herpes remains a prevalent and impactful infection, with ongoing research and advancements in treatment and management. Key developments in the field of herpes research include:
- Improved antiviral medications and treatment options to manage symptoms and reduce the frequency of outbreaks.
- Increased awareness and education efforts to reduce stigma and promote accurate information about herpes.
- Ongoing research into potential vaccines and preventive measures to reduce the incidence of herpes infections.
As research and awareness continue to evolve, individuals can benefit from improved resources and support for managing herpes and maintaining overall health and well-being.
Frequently Asked Questions About Herpes
- Can herpes be cured?
There is currently no cure for herpes, but antiviral medications can help manage symptoms and reduce the frequency of outbreaks.
- Can herpes be transmitted even if there are no visible sores?
Yes, herpes can be transmitted even when an individual is asymptomatic, as the virus can be present on the skin without causing visible symptoms.
- Is herpes a sign of poor hygiene?
No, herpes is a viral infection that can affect anyone, regardless of their hygiene practices. It is transmitted through direct contact with an infected person's skin or bodily fluids.
- Can herpes affect pregnancy?
Yes, herpes can pose risks during pregnancy, particularly if the mother experiences an outbreak near the time of delivery. It's important to work closely with a healthcare provider to manage the infection during pregnancy.
- Are cold sores and genital herpes caused by the same virus?
Cold sores are typically caused by HSV-1, while genital herpes is more commonly associated with HSV-2. However, both types of herpes can cause infections in either location.
- How can I reduce the risk of transmitting herpes to others?
Practicing safe sex, avoiding sexual contact during active outbreaks, and communicating openly with partners can help reduce the risk of transmission.
Conclusion
Herpes 1 vs herpes 2 represents a complex yet vital area of understanding in the realm of viral infections. By recognizing the differences between HSV-1 and HSV-2, individuals can better manage and prevent herpes infections, leading to improved health outcomes and quality of life. Whether it's through treatment, education, or support, navigating the path of living with herpes is achievable with the right resources and knowledge.
For further information and support, individuals are encouraged to consult healthcare professionals and reputable sources to stay informed about the latest developments and strategies in managing herpes effectively.