Urinary tract infections (UTIs) are a common health issue that can cause discomfort and inconvenience to those who experience them. One frequently asked question is whether condoms, typically used to prevent sexually transmitted infections and unwanted pregnancies, could somehow contribute to the development of a UTI. Understanding the relationship between condoms and UTIs is important for anyone who is sexually active and concerned about maintaining good urinary and reproductive health.
Condoms are an essential tool in sexual health, providing a barrier against infections and unintended pregnancies. However, some individuals have reported experiencing UTIs after sexual activity involving condom use. This raises the question: Can condoms cause UTI? By delving into the mechanisms of how UTIs develop, and considering the role of condoms, we can shed light on this topic and offer guidance on how to minimize risks.
In this article, we will explore the potential connection between condom use and UTIs, examine the factors that might influence this relationship, and discuss preventive measures. Our goal is to provide clear, accurate information that empowers individuals to make informed decisions about their sexual health. With expert insights and practical advice, we aim to answer your questions and help you maintain a healthy urinary tract.
Read also:Emily Ratajkowski Tits A Deep Dive Into Her Career And Influence
Table of Contents
- What Are UTIs?
- How Do Condoms Work?
- Can Condoms Cause UTI?
- Factors That Contribute to UTIs
- Types of Condoms and Their Materials
- Allergic Reactions and UTI Risk
- Role of Lubricants in UTI Development
- How to Prevent UTIs While Using Condoms
- Alternative Protection Methods
- Importance of Hydration and Hygiene
- Understanding the Symptoms of UTIs
- When to See a Doctor?
- Treatment Options for UTIs
- Frequently Asked Questions
- Conclusion
What Are UTIs?
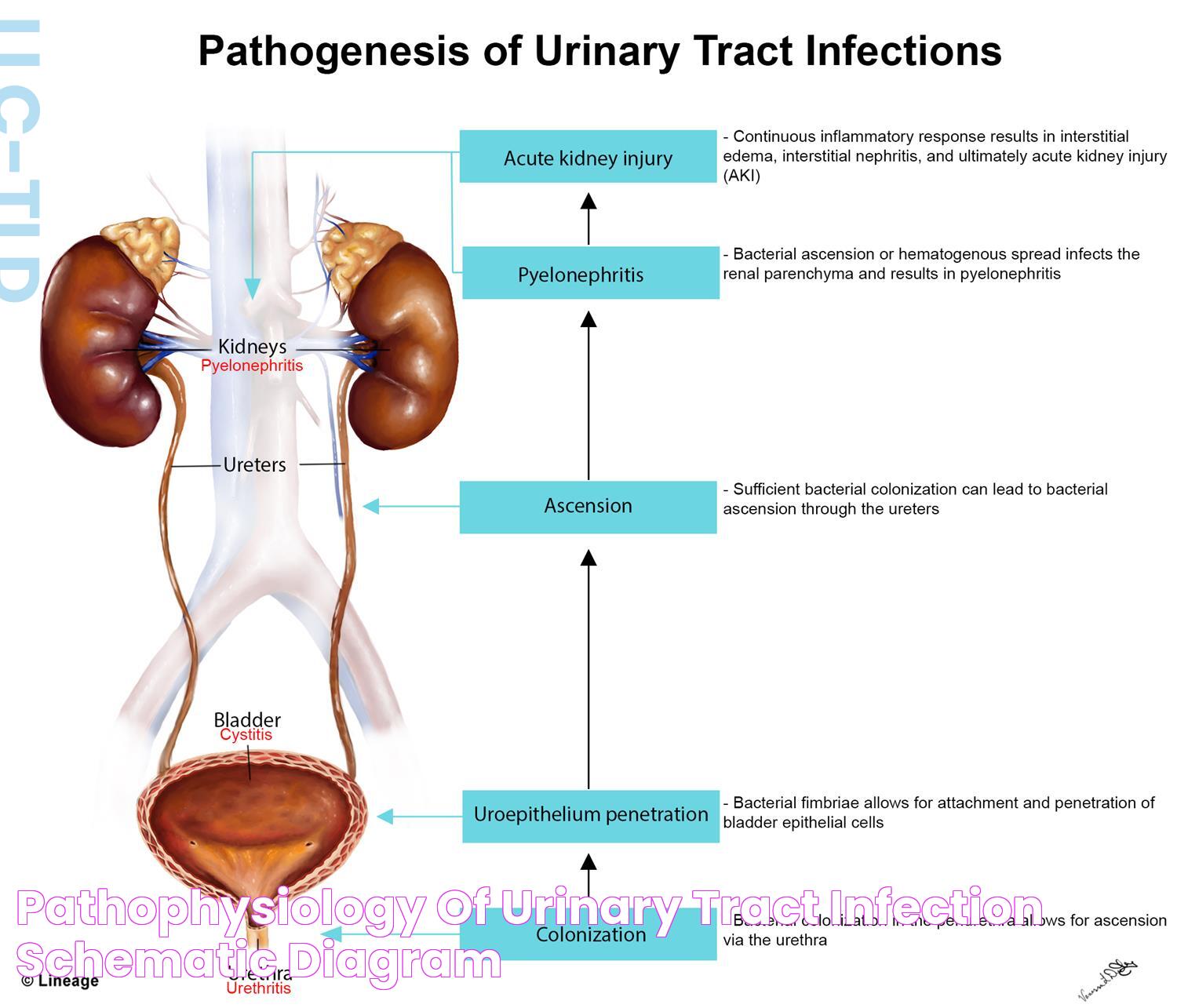
Urinary tract infections (UTIs) are infections that affect any part of the urinary system, including the kidneys, ureters, bladder, and urethra. Most infections involve the lower urinary tract — the bladder and the urethra. Women are at greater risk of developing a UTI than men due to their anatomy.
UTIs occur when bacteria enter the urinary tract through the urethra and begin to multiply in the bladder. While the urinary system is designed to keep out such microscopic invaders, these defenses can sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
Common symptoms of UTIs include a strong, persistent urge to urinate, a burning sensation when urinating, passing frequent, small amounts of urine, and urine that appears cloudy. More severe infections can lead to back pain, fever, and nausea, indicating that the kidneys might be affected.
How Do Condoms Work?
Condoms are barrier devices made from materials such as latex, polyurethane, or lambskin. They are designed to cover the penis or line the vagina during sexual intercourse, preventing bodily fluids, such as semen and vaginal secretions, from mixing. This barrier helps reduce the risk of transmitting sexually transmitted infections (STIs) and prevents pregnancy.
Male condoms are typically made from latex, but there are alternatives for those with latex allergies, such as polyurethane or polyisoprene. Female condoms are made from nitrile and are worn internally. Both types of condoms are effective when used correctly and consistently.
Condoms also come with various features, such as lubrication, ribbing, and flavors, to enhance the sexual experience. They are one of the most accessible and widely used forms of protection worldwide, thanks to their effectiveness and affordability.
Read also:1111 Angel Number Meaning A Guide To Spiritual Significance
Can Condoms Cause UTI?
The question "can condoms cause UTI?" is one that many individuals and couples ponder. While condoms themselves do not directly cause UTIs, certain factors associated with their use may contribute to the development of an infection.
Friction and Irritation
Condom use can sometimes cause friction and irritation during intercourse, particularly if there is insufficient lubrication. This irritation can lead to small abrasions or micro-tears in the vaginal or urethral tissue, potentially facilitating the entry of bacteria into the urinary tract.
Material Sensitivities
Some individuals may be sensitive or allergic to the materials used in condoms, especially latex. This sensitivity can cause irritation and inflammation, which may increase the risk of developing a UTI, as irritated tissues are more susceptible to bacterial invasion.
Improper Use
Improper use of condoms, such as not leaving space at the tip of a male condom or using it inside out, can lead to breakage or spillage, increasing the risk of introducing bacteria into the urethra.
Other Contributing Factors
It's important to note that while condoms are a potential factor, other behaviors and health conditions are more likely to contribute to UTIs, such as sexual activity itself, personal hygiene practices, and individual susceptibility to infections.
Factors That Contribute to UTIs
While condoms can sometimes play a role in the development of a UTI, there are several other factors that commonly contribute to these infections:
- Sexual Activity: Sexual intercourse can introduce bacteria into the urinary tract, particularly for women, due to the proximity of the urethra to the vagina and anus.
- Personal Hygiene: Improper wiping techniques (such as wiping from back to front) can introduce bacteria from the anus into the urethra.
- Use of Spermicides: Spermicides can irritate the skin, increasing the risk of bacterial infection.
- Dehydration: Not drinking enough fluids can lead to infrequent urination, allowing bacteria to accumulate in the urinary tract.
- Underlying Medical Conditions: Conditions such as diabetes and kidney stones can increase the risk of UTIs.
Understanding these factors is crucial in taking preventive steps to reduce the risk of UTIs, regardless of condom use.
Types of Condoms and Their Materials
Condoms come in various types and materials, each with its own benefits and potential drawbacks. The choice of condom can affect comfort, sensitivity, and potential allergic reactions.
Latex Condoms
Latex condoms are the most commonly used type and are highly effective at preventing STIs and pregnancy. They are stretchy and fit snugly, providing a reliable barrier. However, some individuals may be allergic to latex, experiencing irritation or allergic reactions.
Polyurethane and Polyisoprene Condoms
These condoms are excellent alternatives for those with latex allergies. Polyurethane condoms are thinner and offer more sensitivity, while polyisoprene condoms have a similar feel to latex but without the allergenic proteins.
Lambskin Condoms
Made from natural lamb intestines, lambskin condoms are effective for pregnancy prevention but do not protect against STIs, as they have tiny pores that may allow viruses to pass through.
Female Condoms
Female condoms are worn inside the vagina and offer protection similar to male condoms. They provide an option for those who may be allergic to male condom materials or prefer a different method of protection.
Choosing the right type of condom can enhance comfort and reduce the risk of irritation, which may help prevent UTIs.
Allergic Reactions and UTI Risk
Allergic reactions to condoms, particularly those made of latex, can lead to irritation and inflammation, increasing the risk of developing a UTI. Recognizing the signs of an allergic reaction is important for selecting a suitable alternative and minimizing risks.
Signs of a Latex Allergy
Symptoms of a latex allergy may include:
- Itching or redness in the genital area
- Swelling or hives
- Runny nose or sneezing
- Difficulty breathing in severe cases
If you suspect a latex allergy, it's important to switch to non-latex alternatives, such as polyurethane or polyisoprene condoms. Consulting with a healthcare professional can provide further guidance on managing allergies and preventing UTIs.
Role of Lubricants in UTI Development
Lubricants can play a key role in reducing friction during intercourse and preventing irritation. However, certain types of lubricants may increase the risk of UTIs if not chosen carefully.
Water-Based Lubricants
Water-based lubricants are generally safe and compatible with most condoms. They can help reduce friction and the risk of irritation, potentially lowering the chance of a UTI.
Oil-Based Lubricants
Oil-based lubricants, such as petroleum jelly or lotion, can degrade latex condoms and increase the risk of breakage. Additionally, they can cause irritation and may be more likely to contribute to UTIs.
Silicone-Based Lubricants
Silicone-based lubricants are long-lasting and safe to use with latex condoms. They provide a smooth experience and are less likely to contribute to irritation and UTIs.
Choosing the right type of lubricant and ensuring compatibility with your chosen condom can help reduce the risk of UTIs and improve overall comfort during intercourse.
How to Prevent UTIs While Using Condoms
Preventing UTIs while using condoms involves a combination of good hygiene practices, proper condom use, and selecting the right materials and lubricants. Here are some tips to help you minimize the risk:
- Stay Hydrated: Drinking plenty of water helps flush bacteria from the urinary tract.
- Urinate Before and After Intercourse: This helps clear any bacteria that may have been introduced during sexual activity.
- Practice Good Hygiene: Clean the genital area before and after intercourse, and avoid using harsh soaps or douches.
- Choose the Right Condom: Opt for non-latex condoms if you have a latex allergy, and ensure the condom fits properly to prevent irritation.
- Use Compatible Lubricants: Select water-based or silicone-based lubricants to reduce friction and the risk of irritation.
- Follow Proper Condom Usage: Ensure the condom is used correctly, with space at the tip and applied in the right direction.
By following these guidelines, you can reduce the risk of UTIs while maintaining effective protection against STIs and pregnancy.
Alternative Protection Methods
While condoms are a popular choice for protection, there are alternative methods available for those who experience discomfort or UTIs related to condom use. These methods provide varying levels of protection against STIs and pregnancy:
Birth Control Pills
Birth control pills are a hormonal method that prevents pregnancy but do not protect against STIs. They require a prescription and consistent daily use to be effective.
IUDs (Intrauterine Devices)
IUDs are long-term, reversible contraceptive devices inserted into the uterus. They provide effective pregnancy prevention but do not protect against STIs.
Diaphragms
Diaphragms are barrier methods that fit over the cervix to block sperm. They require use with spermicide and offer limited STI protection.
Vaccinations
Vaccinations, such as the HPV vaccine, can protect against certain sexually transmitted infections. They are an important preventive measure for sexual health.
Consulting with a healthcare professional can help determine the best protection method for your individual needs and circumstances.
Importance of Hydration and Hygiene
Maintaining proper hydration and hygiene is essential for preventing UTIs and promoting overall urinary health. These practices can significantly reduce the risk of infection:
Hydration
Staying well-hydrated helps dilute urine and ensures regular urination, flushing bacteria from the urinary tract. Aim to drink at least 8 glasses of water daily, and adjust based on activity level and climate.
Hygiene Practices
Good hygiene practices can prevent the introduction of bacteria into the urinary tract. Key practices include:
- Wiping from front to back after using the toilet to prevent bacteria spread
- Washing the genital area with mild soap and water, avoiding harsh chemicals
- Wearing breathable, cotton underwear to allow airflow and reduce moisture buildup
By incorporating these habits into your daily routine, you can support urinary health and reduce the risk of UTIs.
Understanding the Symptoms of UTIs
Recognizing the symptoms of a UTI is important for seeking prompt treatment and preventing complications. Common symptoms include:
- Strong, persistent urge to urinate
- Burning sensation during urination
- Passing frequent, small amounts of urine
- Cloudy or strong-smelling urine
- Pain or pressure in the lower abdomen or back
In severe cases, symptoms may include fever, chills, nausea, or vomiting, indicating a possible kidney infection. If you experience any of these symptoms, it's important to consult a healthcare professional for evaluation and treatment.
When to See a Doctor?
While mild UTIs may resolve on their own, it's important to seek medical attention under certain circumstances:
- If symptoms persist or worsen after a few days
- If you have recurrent UTIs or underlying health conditions
- If you experience severe symptoms, such as fever or back pain
- If you are pregnant, as UTIs can pose risks to both mother and baby
A healthcare professional can provide appropriate diagnosis and treatment, which may include antibiotics or other interventions.
Treatment Options for UTIs
Treatment for UTIs typically involves antibiotics to eliminate the infection. The choice of antibiotic and duration of treatment depend on the severity of the infection and individual health factors.
Antibiotics
Common antibiotics used to treat UTIs include trimethoprim-sulfamethoxazole, nitrofurantoin, and fosfomycin. It's important to complete the full course of antibiotics as prescribed, even if symptoms improve, to ensure the infection is fully eradicated.
Supportive Care
In addition to antibiotics, supportive care can help alleviate symptoms and promote recovery:
- Drinking plenty of water to flush out bacteria
- Using a heating pad to relieve discomfort
- Taking over-the-counter pain relievers, such as ibuprofen, for pain management
Consulting with a healthcare provider is essential for determining the appropriate treatment plan for your specific situation.
Frequently Asked Questions
1. Can condoms cause UTI?
While condoms themselves do not directly cause UTIs, certain factors related to their use, such as friction or material allergies, may contribute to the risk.
2. What can I do to prevent UTIs when using condoms?
Practicing good hygiene, staying hydrated, using compatible lubricants, and choosing the right type of condom can help prevent UTIs.
3. Are there non-latex condoms available for those with allergies?
Yes, there are non-latex options such as polyurethane and polyisoprene condoms for individuals with latex allergies.
4. How do I know if I have a UTI?
Common symptoms of UTIs include a persistent urge to urinate, burning sensation during urination, and cloudy urine.
5. When should I see a doctor for a UTI?
Seek medical attention if symptoms persist, worsen, or if you experience severe symptoms such as fever or back pain.
6. What treatments are available for UTIs?
UTIs are typically treated with antibiotics, and supportive care such as hydration and pain management can aid recovery.
Conclusion
Understanding the relationship between condom use and the risk of UTIs is crucial for maintaining both sexual and urinary health. While condoms do not directly cause UTIs, certain factors associated with their use can contribute to the risk. By practicing good hygiene, choosing the right materials, and following proper condom usage, you can minimize the likelihood of developing a UTI.
It's important to be informed about the various types of condoms, potential allergic reactions, and the role of lubricants in UTI prevention. Additionally, exploring alternative protection methods may be beneficial for individuals with specific concerns. Ultimately, staying hydrated, recognizing UTI symptoms, and seeking timely medical attention are key components of maintaining urinary health.
By staying informed and proactive, you can enjoy the benefits of safe sexual practices while reducing the risk of urinary tract infections. Remember, consulting with healthcare professionals can provide personalized advice and guidance tailored to your needs.