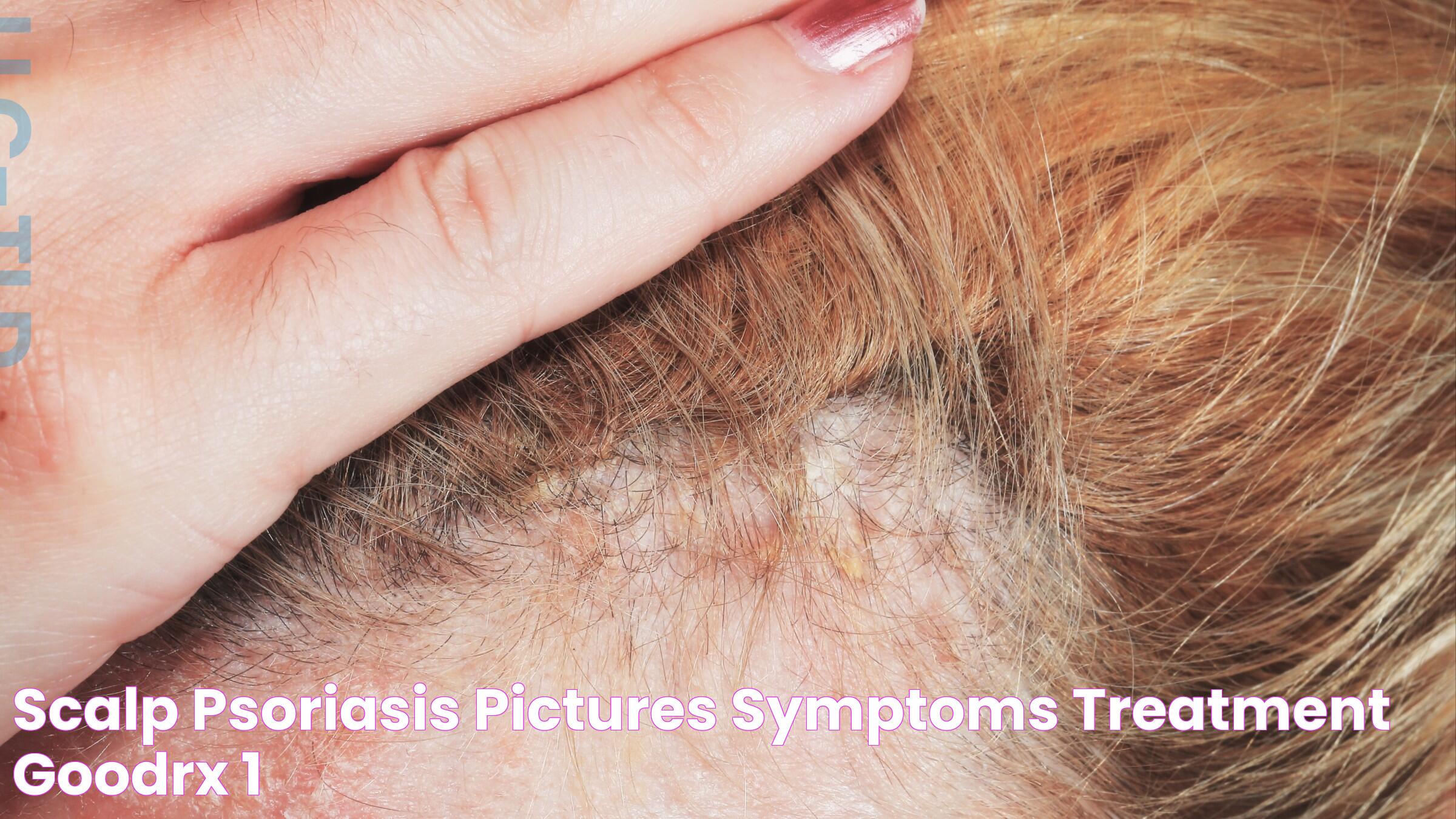
Scalp psoriasis is a chronic skin condition that affects millions of people worldwide, characterized by red, itchy, and scaly patches on the scalp. This condition not only causes physical discomfort but can also have a significant impact on a person's emotional and social well-being. Understanding the symptoms, triggers, and treatment options for scalp psoriasis is crucial for managing this condition effectively.
Psoriasis on the scalp can range from mild, with slight scaling, to severe, where thick, crusted lesions cover the entire scalp. While it may occur in isolation, scalp psoriasis often accompanies psoriasis elsewhere on the body. It is important to differentiate scalp psoriasis from other scalp conditions, such as dandruff or seborrheic dermatitis, to ensure proper treatment. The causes of scalp psoriasis are not entirely understood, but genetic factors, immune system dysfunction, and environmental triggers play a role in its development.
Fortunately, there are various treatment options available for managing scalp psoriasis, from topical treatments to systemic therapies. Lifestyle changes and home remedies can also help alleviate symptoms and prevent flare-ups. While there is no cure for scalp psoriasis, a combination of treatments and self-care strategies can help individuals lead a more comfortable and confident life. This comprehensive guide will explore the intricacies of scalp psoriasis and provide actionable insights for those affected by this condition.
Read also:Net Worth Of Kardashian A Wealthy Legacy
Table of Contents
- What is Scalp Psoriasis?
- Symptoms and Signs of Scalp Psoriasis
- Causes and Risk Factors
- How is Scalp Psoriasis Diagnosed?
- Treatment Options for Scalp Psoriasis
- Topical Treatments
- Systemic Medications and Biologics
- Phototherapy
- Home Remedies and Lifestyle Changes
- Can Diet Impact Scalp Psoriasis?
- Preventing Scalp Psoriasis Flare-Ups
- Living with Scalp Psoriasis
- Does Scalp Psoriasis Affect Mental Health?
- Frequently Asked Questions
- Conclusion
What is Scalp Psoriasis?
Scalp psoriasis is a form of psoriasis where red, scaly patches appear on the scalp. This condition is a chronic autoimmune disorder, meaning the body's immune system mistakenly attacks healthy skin cells. The result is an overproduction of skin cells, leading to the formation of the characteristic plaques. These plaques can be itchy, painful, and may even crack and bleed.
Unlike some other forms of psoriasis, scalp psoriasis can be particularly challenging to manage due to the presence of hair, which can make the application of topical treatments more difficult. Moreover, the visibility of the condition often leads to social anxiety and embarrassment. Despite these challenges, understanding scalp psoriasis is the first step towards effective management and treatment.
Symptoms and Signs of Scalp Psoriasis
Scalp psoriasis symptoms can vary in severity, but common signs include:
- Red patches of skin covered with thick, silvery-white scales.
- Flaky skin resembling dandruff.
- Dry scalp causing itching, soreness, or burning sensations.
- Temporary hair loss due to excessive scratching or removal of scales.
- Bleeding from cracked skin in severe cases.
It is not uncommon for scalp psoriasis to extend beyond the hairline, affecting the forehead, back of the neck, and behind the ears. The severity of symptoms can fluctuate, with periods of remission and flare-ups. Identifying the early signs of scalp psoriasis can lead to timely intervention and better management of the condition.
Causes and Risk Factors
While the exact cause of scalp psoriasis is not fully understood, several factors contribute to its development:
- Genetic predisposition: A family history of psoriasis or other autoimmune diseases increases the risk.
- Immune system dysfunction: An overactive immune response causes rapid skin cell growth.
- Environmental triggers: Stress, infections, and skin injuries can trigger or worsen symptoms.
- Weather conditions: Cold, dry weather can exacerbate symptoms.
- Lifestyle factors: Smoking and heavy alcohol consumption are known risk factors.
Understanding these risk factors can help individuals take preventive measures and manage their condition more effectively. While genetics play a significant role, lifestyle choices and environmental factors can also impact the severity and frequency of scalp psoriasis flare-ups.
Read also:Ultimate Guide To Ulta 21 Days Of Beauty Beauty Event Essentials
How is Scalp Psoriasis Diagnosed?
Diagnosis of scalp psoriasis is typically conducted through a physical examination by a dermatologist. In some cases, a skin biopsy may be performed to rule out other skin conditions. During the examination, the dermatologist will look for the characteristic signs of psoriasis, such as red patches and silvery scales. They may also inquire about family history and any known triggers of flare-ups.
It's important to differentiate scalp psoriasis from other scalp conditions, such as seborrheic dermatitis, as treatment approaches may differ. Accurate diagnosis is crucial for developing an effective treatment plan tailored to the individual's specific needs and symptoms.
Treatment Options for Scalp Psoriasis
There is no one-size-fits-all treatment for scalp psoriasis, and the approach often involves a combination of therapies. The main goal is to reduce inflammation, slow down the growth of skin cells, and remove scales. Treatment options include:
- Topical treatments: Medications applied directly to the scalp.
- Systemic medications: Oral or injectable drugs that affect the entire body.
- Phototherapy: Light therapy to reduce symptoms.
- Home remedies and lifestyle changes: Natural treatments and behavioral adjustments.
Each treatment has its own set of benefits and potential side effects. Consulting with a dermatologist is essential to determine the most appropriate treatment plan based on the severity of the condition and individual preferences.
Topical Treatments
Topical treatments are often the first line of defense against scalp psoriasis. These treatments are applied directly to the affected areas and can be effective in reducing symptoms. Common topical treatments include:
- Corticosteroids: These anti-inflammatory medications help reduce redness and swelling. They come in various forms, including creams, ointments, and shampoos.
- Vitamin D analogs: Synthetic forms of vitamin D that slow down skin cell growth.
- Coal tar: A traditional treatment that reduces scaling, itching, and inflammation.
- Salicylic acid: Helps remove scales and soften the skin.
While topical treatments can be effective, they may require consistent use and proper application techniques to achieve the best results. It's important to follow the dermatologist's instructions and monitor for any adverse reactions.
Systemic Medications and Biologics
For moderate to severe scalp psoriasis, systemic medications may be prescribed. These medications work throughout the body to control inflammation. Common systemic treatments include:
- Oral retinoids: Help normalize skin cell growth.
- Cyclosporine: Suppresses the immune system to reduce symptoms.
- Biologics: Target specific parts of the immune system. These are often used when other treatments have failed.
Biologics are a newer class of drugs that have shown promise in treating psoriasis by targeting specific immune pathways. However, they are typically reserved for more severe cases due to their cost and potential side effects.
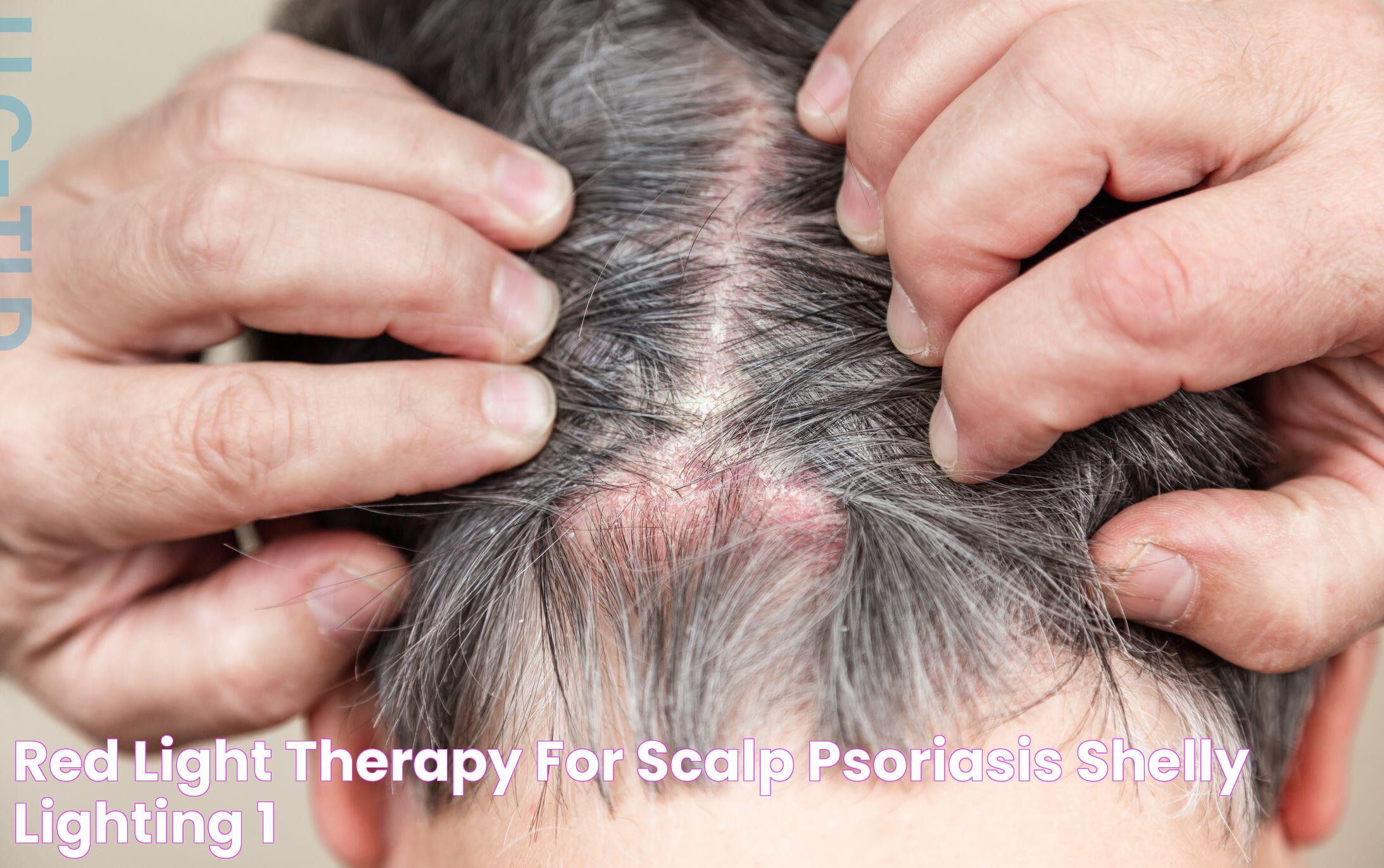
Phototherapy
Phototherapy, or light therapy, involves exposing the skin to ultraviolet light under medical supervision. This treatment can help reduce the severity of scalp psoriasis by slowing down skin cell growth and reducing inflammation. Types of phototherapy include:
- UVB phototherapy: Uses ultraviolet B light to treat psoriasis.
- PUVA therapy: Combines psoralen medication with UVA light.
Phototherapy is usually considered when topical treatments are ineffective or impractical. It requires multiple sessions and can be time-consuming, but many patients find it beneficial in managing their symptoms.
Home Remedies and Lifestyle Changes
In addition to medical treatments, several home remedies and lifestyle changes can help manage scalp psoriasis symptoms:
- Moisturizing: Regularly applying moisturizer can help keep the scalp hydrated and reduce dryness and itching.
- Gentle hair care: Avoid harsh shampoos and minimize the use of hair styling products that can irritate the scalp.
- Stress management: Stress is a known trigger for psoriasis flare-ups. Techniques such as yoga, meditation, and deep breathing exercises can help manage stress levels.
- Diet and nutrition: A balanced diet rich in anti-inflammatory foods may help reduce symptoms.
While these remedies may not cure scalp psoriasis, they can complement medical treatments and improve overall quality of life.
Can Diet Impact Scalp Psoriasis?
Diet may play a role in managing scalp psoriasis, although more research is needed to establish definitive dietary guidelines. Some individuals find that certain foods exacerbate their symptoms, while others report improvements with dietary changes. Common dietary considerations include:
- Anti-inflammatory foods: Incorporating foods like fatty fish, nuts, and leafy greens may help reduce inflammation.
- Avoiding trigger foods: Some people benefit from avoiding foods such as gluten, dairy, or alcohol.
- Omega-3 fatty acids: Found in fish oil, these have anti-inflammatory properties and may benefit psoriasis patients.
It's important to note that dietary changes should complement, not replace, medical treatments. Consulting with a healthcare provider or nutritionist can help develop a personalized dietary plan.
Preventing Scalp Psoriasis Flare-Ups
While it may be impossible to prevent scalp psoriasis entirely, certain strategies can help reduce the frequency and severity of flare-ups:
- Avoid known triggers: Identify and avoid personal triggers, such as stress, certain foods, or harsh hair care products.
- Maintain a consistent treatment regimen: Follow prescribed treatments and keep up with regular dermatologist appointments.
- Protect the scalp: Use hats and scarves in harsh weather conditions to protect the scalp from environmental stressors.
- Stay informed: Keep up with the latest research and treatment options for scalp psoriasis.
By taking proactive measures, individuals with scalp psoriasis can better manage their condition and minimize the impact on their daily lives.
Living with Scalp Psoriasis
Living with scalp psoriasis can be challenging, but with the right strategies, individuals can lead fulfilling lives. Building a support network, whether through friends, family, or psoriasis support groups, can provide emotional support and practical advice. Additionally, practicing self-care and maintaining a positive outlook are essential components of managing a chronic condition.
Educating oneself and others about scalp psoriasis can help reduce stigma and promote understanding. Open communication with healthcare providers, as well as staying informed about new treatments and lifestyle strategies, can empower individuals to take control of their health and well-being.
Does Scalp Psoriasis Affect Mental Health?
Scalp psoriasis can have a significant impact on mental health, leading to feelings of embarrassment, anxiety, and depression. The visible nature of the condition, along with discomfort and itching, can affect self-esteem and social interactions. It's important to address mental health concerns as part of a comprehensive approach to managing scalp psoriasis.
Seeking support from mental health professionals, joining support groups, or participating in therapy can help individuals cope with the emotional aspects of living with scalp psoriasis. Practicing mindfulness and stress-reduction techniques can also contribute to improved mental well-being.
Frequently Asked Questions
1. Can scalp psoriasis lead to permanent hair loss?
Scalp psoriasis itself does not cause permanent hair loss, but excessive scratching or improper treatment can lead to temporary hair shedding. Once the scalp is properly treated and inflammation is reduced, hair usually regrows.
2. Is scalp psoriasis contagious?
No, scalp psoriasis is not contagious. It is an autoimmune condition and cannot be spread from person to person through contact.
3. Can children develop scalp psoriasis?
Yes, children can develop scalp psoriasis. It is important for parents to seek medical advice if they notice symptoms in their child, as early diagnosis and treatment can prevent complications.
4. Are there any natural remedies for scalp psoriasis?
While natural remedies like aloe vera, apple cider vinegar, and tea tree oil may provide some relief, they should not replace medical treatments. Always consult with a healthcare provider before trying new remedies.
5. Can scalp psoriasis affect other parts of the body?
Yes, scalp psoriasis can be part of a more generalized form of psoriasis that affects other areas of the body, such as elbows, knees, and lower back.
6. How long does it take for treatments to show results?
The time it takes for treatments to show results varies depending on the severity of the condition and the specific treatment used. Some people may see improvements within a few weeks, while others may take longer.
Conclusion
Scalp psoriasis is a complex condition that requires a comprehensive approach to management. By understanding the symptoms, triggers, and treatment options, individuals can take control of their condition and improve their quality of life. While there is no cure, a combination of medical treatments, lifestyle changes, and supportive care can help manage symptoms and prevent flare-ups. It's important to work closely with healthcare providers to develop a personalized treatment plan and to address any mental health concerns that may arise as a result of living with scalp psoriasis.
Ultimately, the key to managing scalp psoriasis lies in staying informed, being proactive in treatment and self-care, and seeking support when needed. With the right strategies, those affected by scalp psoriasis can lead healthy, fulfilling lives.