PMS migraine can be an overwhelming experience for many individuals, disrupting daily life and causing significant discomfort. These headaches, often occurring during the premenstrual phase, are not just typical migraines; they are influenced by hormonal changes, making them particularly challenging. Understanding the root causes and effective management strategies is crucial for those affected.
The complexity of PMS migraine lies in its association with the menstrual cycle, which introduces additional variables that can exacerbate or trigger migraine attacks. Many women experience these migraines as part of their premenstrual syndrome (PMS), accompanied by other symptoms such as mood swings, bloating, and fatigue. Addressing PMS migraine requires a multifaceted approach that considers these hormonal fluctuations and their impact on the body.
For those struggling with PMS migraine, finding relief is a top priority. Fortunately, there are various strategies and treatments available that can help manage and reduce the frequency of these migraines. From lifestyle changes and dietary adjustments to medical interventions and alternative therapies, there are many avenues to explore. This guide will delve into the causes, symptoms, and treatment options for PMS migraine, providing a comprehensive resource for those seeking to alleviate this debilitating condition.
Read also:Wrinkle Face A Comprehensive Guide To Understanding And Tackling Aging Skin
Table of Contents
- What Are PMS Migraines?
- Causes of PMS Migraine
- Symptoms of PMS Migraine
- How to Diagnose PMS Migraine?
- Lifestyle Changes for PMS Migraine
- Dietary Considerations
- Medical Treatments
- Alternative Therapies
- Coping Strategies
- PMS Migraine and Mental Health
- How Can Support Systems Help?
- Prevention Tips
- Frequently Asked Questions
- Conclusion
What Are PMS Migraines?
PMS migraines are headaches linked to the menstrual cycle, specifically occurring in the premenstrual phase. They differ from regular migraines due to the hormonal changes that occur during this time. These migraines are often more severe and can be accompanied by other PMS symptoms.
Characteristics of PMS Migraines
PMS migraines typically occur due to hormonal fluctuations, primarily the drop in estrogen levels before menstruation. They can manifest as throbbing pain on one side of the head, sensitivity to light and sound, and nausea.
How Common Are They?
Research indicates that approximately 60% of women who suffer from migraines report an increase in frequency and severity of attacks during menstruation. This highlights the need for targeted treatment strategies for those affected by PMS migraines.
Causes of PMS Migraine
The primary cause of PMS migraine is the hormonal changes that occur during the menstrual cycle. The sudden drop in estrogen levels just before menstruation is a significant trigger for these migraines. Additionally, other factors such as stress, lack of sleep, and dietary habits can contribute to the onset of PMS migraines.
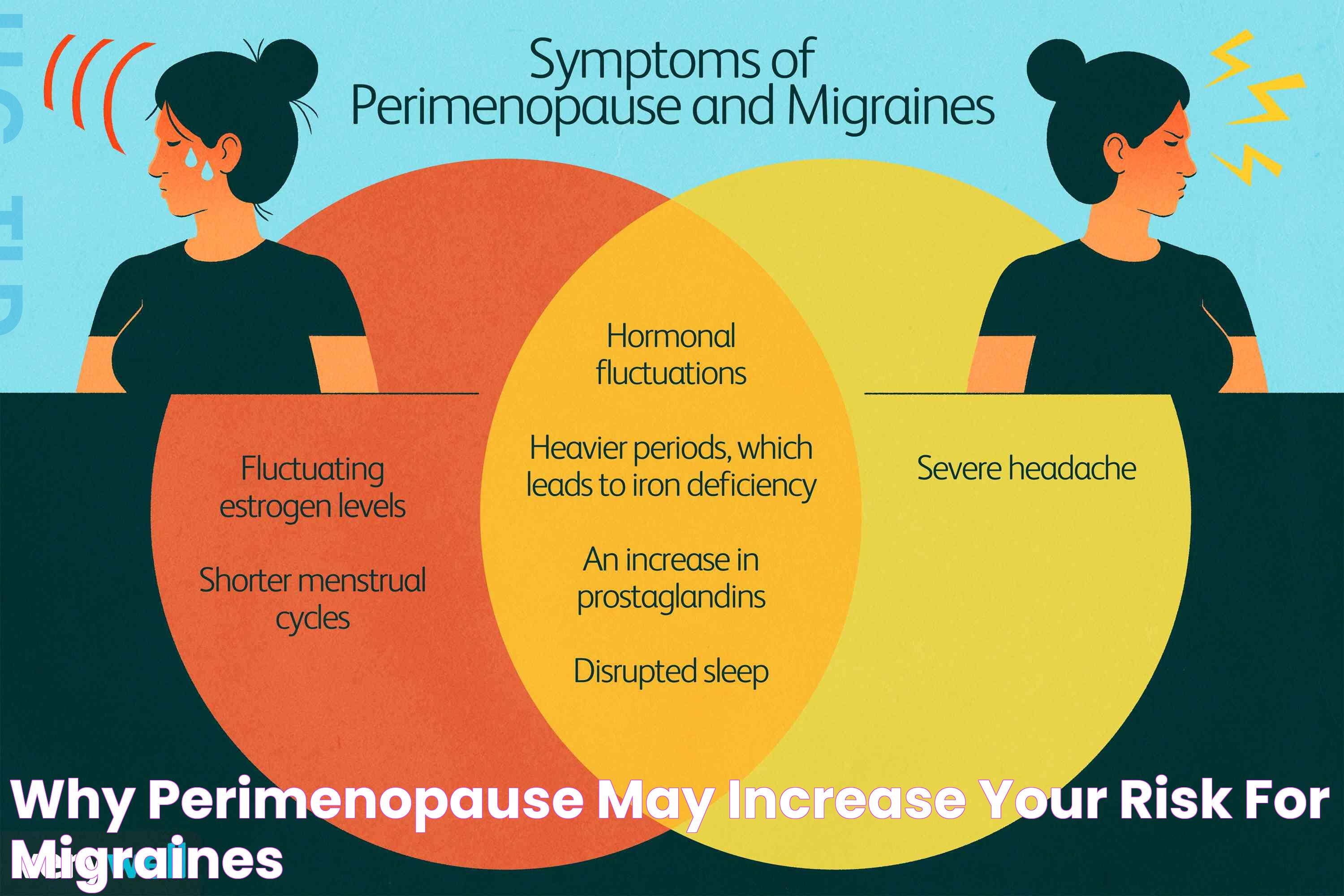
Hormonal Fluctuations
During the menstrual cycle, the levels of estrogen and progesterone fluctuate. The decrease in estrogen levels right before a period is often linked to the onset of PMS migraine. This hormonal trigger can make the brain more sensitive to other migraine triggers.
Other Contributing Factors
- Stress: Emotional stress can exacerbate hormonal changes, leading to migraines.
- Diet: Certain foods and drinks, such as caffeine and alcohol, can trigger migraines.
- Lack of Sleep: Irregular sleep patterns can increase the likelihood of migraines.
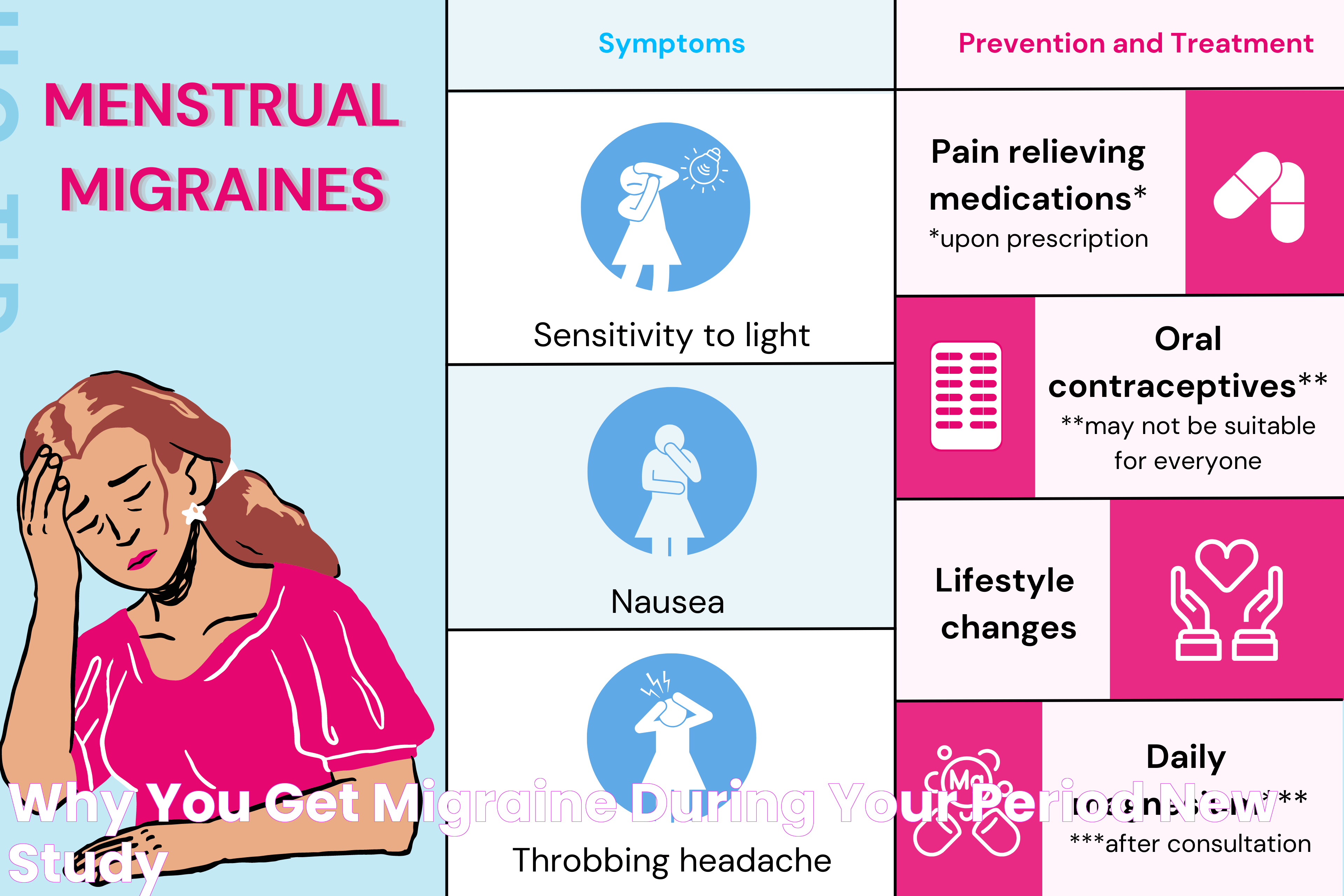
Symptoms of PMS Migraine
The symptoms of PMS migraine are similar to those of regular migraines but can be more intense due to the hormonal context. They include:
Read also:Top Picks For Good Teeth Whitening Toothpaste Effective And Safe Options
- Throbbing or pulsing headache, often on one side of the head
- Sensitivity to light, sound, and sometimes smell
- Nausea and vomiting
- Dizziness or vertigo
Additional PMS Symptoms
Alongside migraine symptoms, individuals may experience other PMS-related symptoms such as:
- Mood swings and irritability
- Bloating and abdominal cramps
- Fatigue and sleep disturbances
How to Diagnose PMS Migraine?
Diagnosing PMS migraine involves a comprehensive evaluation by a healthcare professional. It includes reviewing medical history, symptoms, and identifying any patterns related to the menstrual cycle.
Medical History and Headache Diary
Keeping a headache diary can help identify patterns and triggers. This record should include the timing, duration, and intensity of the headaches, along with any associated symptoms and potential triggers.
Consultation with a Healthcare Provider
A healthcare provider may conduct a physical exam and possibly recommend tests to rule out other conditions. They may also inquire about menstrual cycle patterns to establish a link between migraines and hormonal changes.
Lifestyle Changes for PMS Migraine
Adopting certain lifestyle changes can significantly reduce the frequency and severity of PMS migraines. These changes focus on maintaining hormonal balance and minimizing triggers.
Regular Exercise
Engaging in regular physical activity can help regulate hormones and reduce stress, which may alleviate PMS migraine symptoms.
Stress Management Techniques
- Meditation and deep breathing exercises
- Practicing yoga or tai chi
- Engaging in hobbies and relaxation activities
Dietary Considerations
Diet plays a crucial role in managing PMS migraines. Certain foods can trigger migraines, while others may help prevent them.
Foods to Avoid
- Caffeine and alcohol
- Processed foods and artificial sweeteners
- Foods high in sodium and sugar
Beneficial Foods
- Magnesium-rich foods like leafy greens and nuts
- Foods high in omega-3 fatty acids such as fish and flaxseeds
- Hydrating foods like fruits and vegetables
Medical Treatments
Several medical treatments can help manage PMS migraines. These treatments focus on alleviating symptoms and preventing future attacks.
Over-the-Counter Medications
- Ibuprofen or naproxen for pain relief
- Antiemetics for nausea
Prescription Medications
In some cases, doctors may prescribe medications such as triptans or hormonal therapies to manage PMS migraines more effectively.
Alternative Therapies
Alternative therapies can complement traditional treatments and provide additional relief for PMS migraine sufferers.
Acupuncture
Acupuncture has been shown to reduce the frequency and intensity of migraines by promoting relaxation and balancing the body's energy flow.
Herbal Remedies
- Feverfew and butterbur supplements
- Ginger for nausea relief
Coping Strategies
Developing effective coping strategies can help individuals manage PMS migraines and improve their quality of life.
Mindfulness and Relaxation Techniques
- Practicing mindfulness meditation
- Using guided imagery or progressive muscle relaxation
Support Groups
Joining support groups can provide emotional support and practical advice from others who experience PMS migraines.
PMS Migraine and Mental Health
The impact of PMS migraines extends beyond physical symptoms, affecting mental health and emotional well-being.
Understanding the Connection
Chronic pain and discomfort from migraines can lead to anxiety and depression. Addressing these mental health issues is crucial for comprehensive migraine management.
Therapeutic Approaches
- Cognitive-behavioral therapy (CBT)
- Stress management and relaxation training
How Can Support Systems Help?
Support systems play a vital role in managing PMS migraines by providing emotional and practical support.
Family and Friends
Having a supportive network of family and friends can help individuals cope with the challenges of PMS migraines. They can assist with daily tasks and offer emotional comfort.
Healthcare Professionals
Regular consultations with healthcare professionals can ensure appropriate treatment and management of PMS migraines.
Prevention Tips
Preventing PMS migraines involves a proactive approach to managing triggers and maintaining a healthy lifestyle.
Consistent Sleep Schedule
- Maintain a regular sleep routine
- Create a relaxing bedtime environment
Hydration and Nutrition
- Drink plenty of water throughout the day
- Follow a balanced diet with adequate nutrients
Frequently Asked Questions
- What triggers PMS migraines?
Hormonal changes, stress, certain foods, and lack of sleep are common triggers for PMS migraines.
- Can lifestyle changes help reduce PMS migraines?
Yes, regular exercise, stress management, and a healthy diet can help reduce the frequency and severity of PMS migraines.
- What medications are effective for PMS migraines?
OTC medications like ibuprofen, prescription triptans, and hormonal therapies can be effective in managing PMS migraines.
- Are there alternative therapies for PMS migraines?
Yes, acupuncture, herbal remedies, and mindfulness techniques can complement traditional treatments for PMS migraines.
- How does PMS migraine affect mental health?
PMS migraines can lead to anxiety and depression, highlighting the importance of addressing mental health alongside physical symptoms.
- What role do support systems play in managing PMS migraines?
Support systems provide emotional and practical support, helping individuals cope with the challenges of PMS migraines.
Conclusion
PMS migraine is a complex condition influenced by hormonal changes and various triggers. By understanding the causes and exploring a range of management strategies, individuals can find relief from these debilitating headaches. From lifestyle modifications and dietary adjustments to medical treatments and alternative therapies, there are numerous options available to help manage PMS migraines. With the right approach and support, it is possible to reduce the impact of PMS migraines and improve overall quality of life.
For more information and resources on PMS migraines, consider visiting reputable health websites such as Mayo Clinic.