Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. It is characterized by a range of symptoms that can significantly impact an individual's daily life, mental health, and overall well-being. Understanding the symptoms of PTSD is crucial for those affected and their loved ones, as it can lead to earlier diagnosis, effective treatment, and better coping strategies.
Living with PTSD can be a daunting experience, but recognizing the symptoms is the first step toward healing. People with PTSD might experience flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the traumatic event. These symptoms can be distressing and overwhelming, affecting an individual's ability to function normally in everyday situations. Fortunately, with the right support and treatment, those with PTSD can learn to manage their symptoms and lead fulfilling lives.
In this article, we will delve into the symptoms of PTSD, explore their causes, and discuss available treatment options. We'll also provide insights into coping mechanisms and support systems that can aid in recovery. Whether you are personally affected by PTSD or supporting someone who is, this guide aims to equip you with the knowledge and tools to navigate this challenging condition.
Read also:Longevity Of False Eyelashes Tips Amp Insights For Lasting Beauty
Table of Contents:
- What is PTSD?
- Recognizing PTSD Symptoms
- How Does PTSD Manifest?
- Intrusive Thoughts and Flashbacks
- Nightmares and Sleep Disorders
- Emotional Numbing and Detachment
- Hyperarousal and Irritability
- Understanding the Triggers
- How to Diagnose PTSD?
- Treatment Options for PTSD
- How Can You Support Someone with PTSD?
- Coping Strategies for PTSD
- Can PTSD Be Prevented?
- Living with PTSD Long-term
- FAQs about Symptoms of PTSD
- Conclusion
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a psychiatric disorder that can occur in individuals who have experienced or witnessed a traumatic event such as a natural disaster, a serious accident, a terrorist act, war/combat, rape or other violent personal assault. PTSD can affect anyone, regardless of their age, gender, or background.
PTSD is classified as an anxiety disorder, and it can significantly impair a person's ability to function in daily life. It is characterized by intense, disturbing thoughts and feelings related to the traumatic experience that last long after the traumatic event has ended. People with PTSD may relive the event through flashbacks or nightmares, may feel sadness, fear or anger, and may feel detached or estranged from others. They may avoid situations or people that remind them of the traumatic event, and they may have strong negative reactions to something as ordinary as a loud noise or an accidental touch.
PTSD was once known as "shell shock" or "combat fatigue" following World War I and II, but it has been recognized as a formal diagnosis since the 1980s. Today, mental health professionals understand that PTSD is a serious condition that can affect anyone, not just combat veterans. The recognition of PTSD as a legitimate mental health issue has led to significant advancements in treatment and support for those affected.
Recognizing PTSD Symptoms
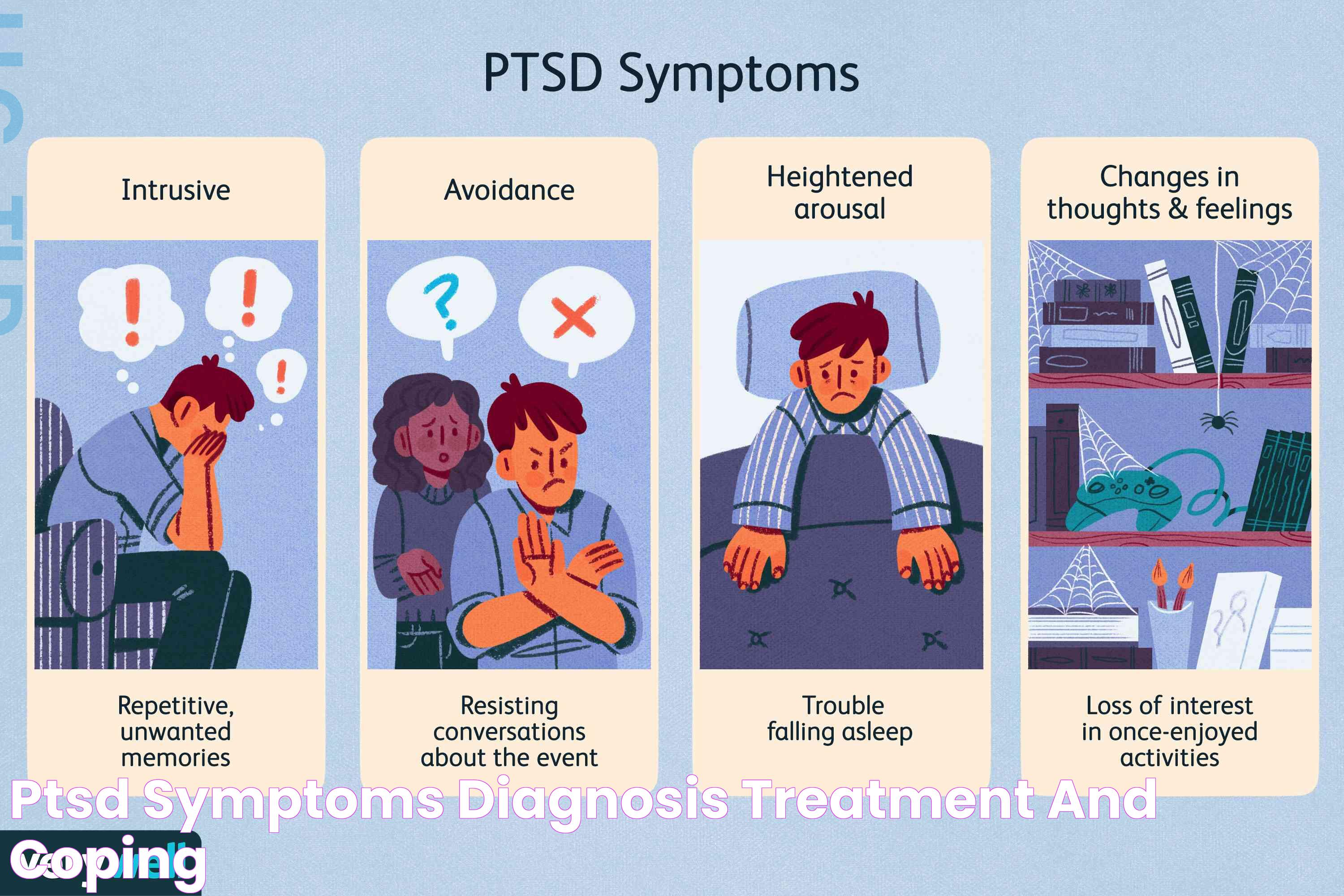
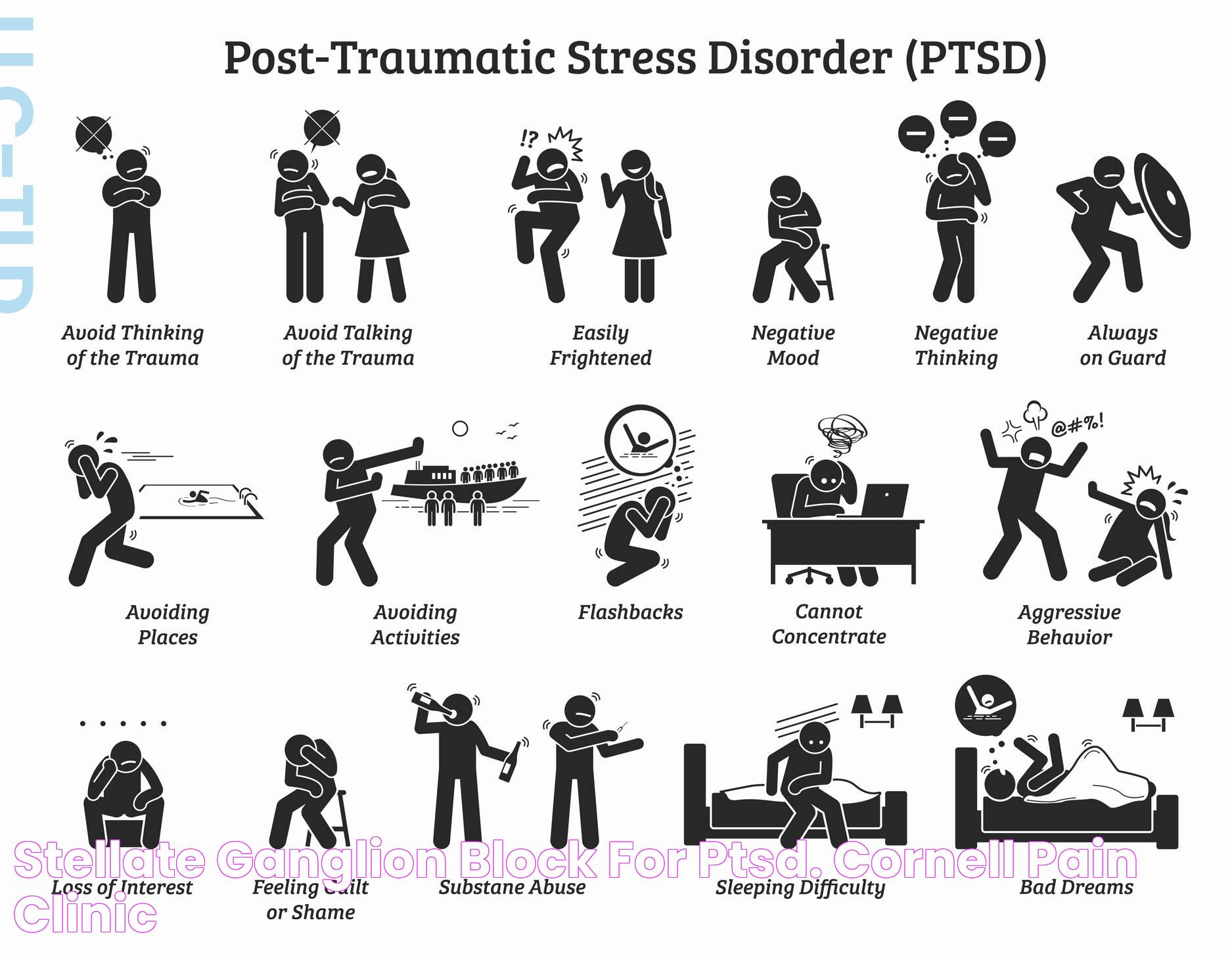
Understanding the symptoms of PTSD is the first step towards identifying and addressing the condition. PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. These symptoms can vary over time and from person to person.
Some common symptoms of PTSD include:
- Intrusive memories: Recurrent, unwanted distressing memories of the traumatic event, flashbacks, or nightmares.
- Avoidance: Trying to avoid thinking or talking about the traumatic event, or avoiding places, activities, or people that remind you of the trauma.
- Negative thoughts and mood: Negative thoughts about yourself, other people, or the world, hopelessness about the future, memory problems, or difficulty maintaining close relationships.
- Changes in physical and emotional reactions: Being easily startled or frightened, always being on guard for danger, self-destructive behavior, or trouble sleeping.
It's important to note that not everyone who experiences a traumatic event will develop PTSD. It's normal to have a range of reactions following trauma, and most people will recover naturally. However, if symptoms persist and interfere with daily life, it may be time to seek professional help.
Read also:Redefining Perception Function Is Beauty In Modern Design
How Does PTSD Manifest?
The manifestation of PTSD can vary widely among individuals, but there are several common patterns and behaviors that may indicate the presence of the disorder. Understanding these manifestations can help in recognizing the condition and seeking appropriate help.
PTSD manifests through a series of emotional, psychological, and physical symptoms, which often occur in clusters. These can include:
- Re-experiencing the trauma through intrusive thoughts, flashbacks, and nightmares. These episodes can be triggered by reminders of the trauma, such as certain sounds, smells, or locations.
- Avoidance of situations or people that trigger memories of the trauma. This can lead to social withdrawal and isolation, as well as a reluctance to engage in activities that were once enjoyable.
- Negative changes in thoughts and mood. This can involve feelings of hopelessness, detachment from friends and family, or a diminished interest in life. Individuals may also experience memory problems or a distorted sense of blame or guilt.
- Heightened physiological arousal, which can manifest as hypervigilance, irritability, difficulty concentrating, or an exaggerated startle response. This state of heightened alertness can interfere with sleep and lead to a sense of being on edge.
These symptoms can be persistent and severe, making it difficult for those with PTSD to carry out day-to-day activities. Recognizing these patterns is crucial for early intervention and effective treatment.
Intrusive Thoughts and Flashbacks
Intrusive thoughts and flashbacks are hallmark symptoms of PTSD, often causing significant distress to those affected. These episodes can be triggered by reminders of the traumatic event, leading to a vivid re-experiencing of the trauma as if it were happening again.
Intrusive thoughts can occur without warning, disrupting daily activities and concentration. They may be accompanied by vivid images, sounds, or smells associated with the trauma. Flashbacks, on the other hand, are more intense and can feel like a complete reliving of the event, often involving a loss of awareness of the present moment.
These symptoms can be frightening and disorienting, making it difficult to distinguish between past and present. Managing intrusive thoughts and flashbacks requires therapeutic interventions such as cognitive-behavioral therapy (CBT) or eye movement desensitization and reprocessing (EMDR), which can help individuals process their traumatic memories and reduce their impact.
Nightmares and Sleep Disorders
Nightmares are a common symptom of PTSD, often involving terrifying dreams related to the traumatic event. These nightmares can lead to severe sleep disturbances, impacting both physical and mental health.
Individuals with PTSD may experience difficulty falling asleep, staying asleep, or achieving restful sleep. This can lead to chronic sleep deprivation, affecting mood, cognitive function, and overall quality of life. The fear of having recurring nightmares may also cause individuals to avoid sleep altogether, exacerbating the problem.
Treatment for sleep disorders associated with PTSD may include medication, therapy, or a combination of both. Cognitive-behavioral therapy for insomnia (CBT-I) is a specialized form of CBT that can help address sleep disturbances by modifying thought patterns and behaviors related to sleep. Relaxation techniques, such as deep breathing or progressive muscle relaxation, can also promote better sleep.
Emotional Numbing and Detachment
Emotional numbing and detachment are symptoms of PTSD that can significantly impact personal relationships and social interactions. Individuals may feel disconnected from their emotions, leading to a sense of isolation and alienation from others.
Emotional numbing may manifest as an inability to experience positive emotions, such as happiness or love. This can result in a diminished interest in activities that were once enjoyable, as well as difficulties in forming or maintaining close relationships.
Detachment from others can stem from a desire to avoid reminders of the trauma or a belief that others cannot understand their experiences. This can lead to withdrawal from social situations and a reluctance to seek support, which can further exacerbate feelings of loneliness and despair.
Overcoming emotional numbing and detachment often involves therapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT), which can help individuals reconnect with their emotions and build meaningful relationships.
Hyperarousal and Irritability
Hyperarousal is a state of heightened alertness and increased sensitivity to potential threats, often experienced by individuals with PTSD. This symptom can manifest as irritability, difficulty concentrating, and an exaggerated startle response.
Those with PTSD may feel constantly on edge, as if they are in a state of perpetual danger. This heightened state of arousal can lead to difficulties in relaxing or unwinding, resulting in chronic stress and anxiety.
Irritability and anger outbursts are common in individuals with PTSD, often triggered by seemingly minor events. These emotional responses can strain relationships and create challenges in professional or social settings.
Managing hyperarousal and irritability may involve a combination of therapy, medication, and relaxation techniques. Mindfulness-based stress reduction (MBSR) and other mindfulness practices can help individuals cultivate a sense of calm and reduce the physiological symptoms of hyperarousal.
Understanding the Triggers
Triggers are external stimuli that can evoke memories and emotions associated with a traumatic event, leading to a resurgence of PTSD symptoms. Understanding and identifying these triggers is essential for managing and alleviating the symptoms of PTSD.
Triggers can be specific to the individual and may include:
- Sensory reminders such as sounds, smells, or images related to the trauma.
- Emotional responses, such as feelings of fear or sadness.
- Situations that resemble or symbolize the traumatic event, such as crowded places for someone who has experienced an attack.
Recognizing these triggers can empower individuals to develop strategies to cope with or avoid them, thereby reducing their impact. This may involve therapy to process traumatic memories and learn coping techniques, as well as developing a strong support network to provide assistance and understanding.
How to Diagnose PTSD?
Diagnosing PTSD involves a comprehensive assessment by a qualified mental health professional, such as a psychiatrist or psychologist. The diagnostic process typically includes a clinical interview, questionnaires, and a review of the individual's symptoms and history.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines the criteria for diagnosing PTSD, which includes exposure to a traumatic event, the presence of specific symptoms, and significant distress or impairment in social, occupational, or other areas of functioning.
The diagnostic process may involve:
- A detailed interview to assess the individual's symptoms, history, and functioning.
- Standardized questionnaires or self-report measures to evaluate the presence and severity of symptoms.
- Collaboration with other healthcare providers to rule out other medical or psychological conditions that may mimic PTSD symptoms.
Early diagnosis and intervention are critical for effective treatment and recovery. If you or someone you know is experiencing symptoms of PTSD, seeking professional help can lead to a better understanding of the condition and appropriate treatment options.
Treatment Options for PTSD
Treatment for PTSD is tailored to the individual's needs and may involve a combination of psychotherapy, medication, and support from healthcare professionals. The goal of treatment is to reduce symptoms, improve functioning, and enhance overall quality of life.
Common treatment options for PTSD include:
- Psychotherapy: Cognitive-behavioral therapy (CBT) is the most effective form of psychotherapy for PTSD, focusing on changing negative thought patterns and behaviors. Other therapeutic approaches include eye movement desensitization and reprocessing (EMDR) and prolonged exposure therapy.
- Medication: Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are commonly prescribed to help manage the symptoms of PTSD. Other medications, such as mood stabilizers or anti-anxiety medications, may be used as needed.
- Support Groups: Peer support groups provide a safe space for individuals with PTSD to share their experiences and learn from others. These groups can offer emotional support, practical advice, and a sense of community.
It's important for individuals with PTSD to work closely with their healthcare providers to develop a personalized treatment plan that addresses their unique needs and goals. Treatment may require time and commitment, but with the right support and resources, recovery is possible.
How Can You Support Someone with PTSD?
Supporting someone with PTSD can be challenging, but understanding their condition and offering empathy and patience can make a significant difference in their recovery journey. Here are some ways to support a loved one with PTSD:
- Educate Yourself: Learn about PTSD and its symptoms to better understand what your loved one is going through. This knowledge can help you provide informed support and avoid unintentional triggers.
- Listen and Validate: Offer a listening ear without judgment, and validate their feelings and experiences. Let them know that you are there for them and that their emotions are valid.
- Encourage Treatment: Encourage your loved one to seek professional help and support them in attending therapy sessions or appointments. Offer to accompany them if they feel comfortable with it.
- Be Patient: Recovery from PTSD takes time, and there may be setbacks along the way. Be patient and understanding, and avoid pressuring them to "move on" or "get over it."
- Promote Self-Care: Encourage healthy habits such as regular exercise, a balanced diet, and sufficient sleep. These activities can help improve mood and overall well-being.
Supporting someone with PTSD requires compassion and understanding. By being present and offering consistent support, you can help your loved one navigate the challenges of PTSD and work towards healing.
Coping Strategies for PTSD
Developing effective coping strategies is essential for managing the symptoms of PTSD and improving quality of life. While professional treatment is crucial, self-help techniques and lifestyle changes can complement therapy and medication.
Some coping strategies for PTSD include:
- Mindfulness and Relaxation: Practice mindfulness meditation, deep breathing exercises, or yoga to help reduce stress and promote relaxation.
- Physical Activity: Engage in regular physical activity, such as walking, jogging, or swimming, to boost mood and reduce anxiety.
- Journaling: Write about your thoughts and feelings to process emotions and gain clarity.
- Social Support: Connect with friends, family, or support groups to share experiences and receive encouragement.
- Limit Triggers: Identify and avoid triggers that exacerbate symptoms, and develop strategies to cope with unavoidable triggers.
By incorporating these coping strategies into daily life, individuals with PTSD can enhance their resilience and improve their ability to manage symptoms. It's important to remember that coping strategies are personal and may require experimentation to find what works best for each individual.
Can PTSD Be Prevented?
While it's not always possible to prevent PTSD, certain strategies can reduce the risk of developing the disorder after a traumatic event. Early intervention and support can play a significant role in mitigating the impact of trauma.
Some preventative measures include:
- Early Intervention: Seeking professional help soon after a traumatic event can help process emotions and reduce the risk of developing PTSD.
- Building Resilience: Developing coping skills, fostering a strong support network, and engaging in stress-reduction activities can enhance resilience and improve the ability to cope with trauma.
- Education and Awareness: Increasing awareness about PTSD and its symptoms can help individuals recognize and address the condition before it worsens.
While not all cases of PTSD can be prevented, taking proactive steps to address trauma and promote mental health can reduce the likelihood of developing the disorder and support recovery.
Living with PTSD Long-term
Living with PTSD long-term can present ongoing challenges, but with the right support and strategies, individuals can lead fulfilling and meaningful lives. Understanding the condition and actively engaging in treatment and self-care are key to managing symptoms over time.
Some considerations for living with PTSD long-term include:
- Maintaining Treatment: Continuing to engage in therapy and follow treatment plans can help manage symptoms and prevent relapses.
- Building a Support System: Surrounding yourself with supportive friends, family, and healthcare providers can provide encouragement and understanding.
- Adapting Coping Strategies: As life circumstances change, so may the need for different coping strategies. Stay open to trying new approaches and adjusting your self-care routine.
- Advocacy and Awareness: Sharing your experiences with PTSD can raise awareness and reduce stigma, helping others understand the condition and seek help.
While PTSD can be a lifelong condition, it does not define an individual. With perseverance and support, individuals with PTSD can achieve recovery and live fulfilling lives.
FAQs about Symptoms of PTSD
1. What are the early warning signs of PTSD?
Early warning signs of PTSD may include experiencing intrusive thoughts, nightmares, or flashbacks related to a traumatic event. Individuals may also exhibit avoidance behaviors, emotional numbness, or heightened anxiety and irritability.
2. Can PTSD symptoms appear years after the traumatic event?
Yes, PTSD symptoms can develop months or even years after the traumatic event. Delayed-onset PTSD is not uncommon, and symptoms may be triggered by a major life change or a reminder of the trauma.
3. Is it possible to have PTSD without experiencing a traumatic event?
PTSD is typically associated with exposure to a traumatic event, but individuals can also experience symptoms of PTSD-like conditions, known as secondary traumatic stress, from indirect exposure, such as hearing about a loved one's trauma.
4. How can I tell if someone has PTSD?
Signs that someone may have PTSD include changes in mood or behavior, increased irritability, avoidance of certain places or activities, and difficulty maintaining relationships. A mental health professional can provide a formal diagnosis.
5. Can PTSD be cured?
While there is no cure for PTSD, with appropriate treatment and support, individuals can manage symptoms and lead fulfilling lives. Recovery is an ongoing process, and many people with PTSD experience significant improvement.
6. What is the role of medication in treating PTSD?
Medication can be an important component of PTSD treatment, helping to alleviate symptoms such as depression and anxiety. Antidepressants, particularly SSRIs, are commonly prescribed, along with other medications as needed.
Conclusion
Understanding the symptoms of PTSD is crucial for recognizing and addressing this complex mental health condition. While living with PTSD can present challenges, early diagnosis, effective treatment, and strong support networks can significantly improve outcomes for those affected. By raising awareness and fostering empathy, we can create a more supportive environment for individuals with PTSD to heal and thrive.
For further resources and support, consider reaching out to mental health organizations, healthcare professionals, or support groups. Remember, recovery is possible, and no one has to face PTSD alone.